Find a Cardiologist
4 Heart Health Tips
Do you know someone who has heart disease? Chances are you do. More than 28 million Americans have been diagnosed with the condition. If you don’t want to join this group, pay attention to these heart health tips to reduce your personal risk of heart disease.
Tip #1: Eat healthy.
A healthy diet includes a variety of grains (especially whole grains), fruits and vegetables. Opt for foods low in saturated and trans fats, cholesterol, added sugar and salt. Choose fish, poultry and lean cuts of meat, as well as low-fat or fat-free dairy products. Limit the number of egg yolks and cut down on processed cold cuts. When preparing food, broil, bake, roast or poach instead of frying, and tame snack attacks with low-fat options, such as animal crackers or fat-free yogurt. Another heart health tip is to limit how much alcohol you drink. Too much alcohol can raise blood pressure (more than two drinks per day for men and one drink per day for women).
Tip #2: Exercise regularly.
As little as 30 minutes of moderate-intensity physical activity on most days of the week is all you need to protect heart health. Don’t like to exercise? No sweat. Good ways to keep your heart healthy include brisk walking, riding a bike, hiking, dancing, swimming, physical tasks around the house, raking leaves or painting a room. Other ways to work exercise into your day include taking the stairs when possible, or parking farther away from the office and then walking the added distance.
Tip #3: Don’t smoke.
According the Centers for Disease Control and Prevention, smoking is “the leading cause of preventable disease, disability and death and disease in the United States.” Compared to nonsmokers, smokers are at an increased risk of heart disease due to the buildup of plaque in their coronary arteries overtime. Quitting smoking can lower the risk of heart disease – and just one year of not smoking may cut heart disease risk in half.
Tip #4: Maintain a healthy weight.
A healthy weight can be calculated by looking at either body mass index (BMI) or waist circumference. BMI, a calculation based on height and weight, of 25 to 29.9 is considered overweight, and 30 or higher is obese. A waist measurement of more than 35 inches for women and 40 inches for men increases the risk of heart disease, high blood pressure and other serious health conditions. A weight loss of just five to 10 percent of current weight can help lower the risk for heart disease. Gradual weight loss of one-half to two pounds per week is recommended to ensure long-term success.
Get Regular Checkups!
In addition to making lifestyle changes, you should also have blood pressure and cholesterol levels checked on a regular basis. Hypertension of 140/90 mmHg or higher is a major risk factor for heart disease that usually does not cause symptoms. Total cholesterol of 240 mg/dL and above is an indication of too much cholesterol that can eventually accumulate on artery walls, making them narrow and impeding blood flow to the heart.
It is important to remember that regardless of your age or current state of health, it is never too late to practice heart health tips to protect your heart. For more information about heart health, talk with your doctor.

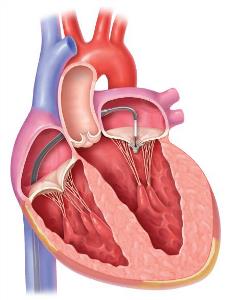 Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing.
Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing. The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.
The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.