Transcatheter Mitral Valve Repair
What is Mitral Regurgitation?
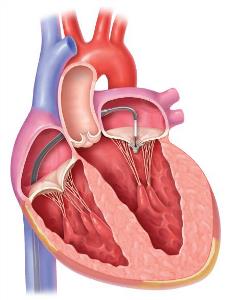
The heart has four valves to ensure that blood flows in one direction through the heart. On the left side of the heart, blood returns with oxygen from the lungs into the left atrium, passes through the mitral valve into the left ventricle, which then pumps blood through the aortic valve to the body. Mitral regurgitation (MR) occurs when the mitral valve fails to close properly, so some of the blood the heart pumps leaks backwards into the left atrium. In rare circumstances, MR may develop acutely and be severe, posing a life-threatening situation. More commonly, it develops gradually and is detected by the presence of a heart murmur. Over time, the heart will enlarge, the back pressure from regurgitant flow will increase pressure in the lung vessels, and an irregular heart beat called atrial fibrillation may develop. With increasing leakage, a patient may develop fatigue and shortness of breath with less activity. Eventually, if left untreated, the left ventricle will become severely dilated and weaker, causing worsening "congestive heart failure" which carries a very poor prognosis.
The mitral valve resembles a parachute with two valve leaflets and strings ("chords") that attach the leaflets to muscles arising from the left ventricular wall ("papillary muscles"). Abnormalities in any of these can cause mitral regurgitation. Surgery has generally been indicated to correct MR when the patient develops symptoms or there is evidence that the heart is becoming significantly enlarged or becomes weaker. In addition, when the lung artery pressure is significantly increased or atrial fibrillation develops, surgery should be considered.
Transcatheter Mitral Valve Repair
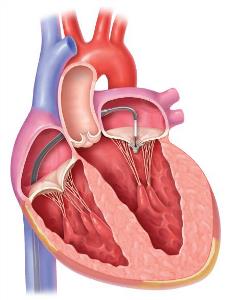 Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing.
Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing.
Am I a Candidate for a MitraClip?
This device is only approved for patients considered at prohibitive risk for surgery because surgery is a much better means of eliminating the MR and is otherwise preferable. Studies in the United States have shown benefit for patients with degenerative MV disease, while studies in Europe show that it is effective for functional disease. The latter indication is not yet approved in the United States, pending results of a large trial. A careful evaluation of your history, medical problems, overall physical condition, and a detailed analysis of your echocardiogram will determine whether the procedure is indicated or feasible. Patients with significant comorbidities, complex mitral valve disease, severe right ventricular dysfunction, and severe tricuspid regurgitation may not benefit from the procedure.
What Should I Expect if My Doctor Recommends an Evaluation for a MitraClip?
If your doctor suspects that you have severe mitral regurgitation, an echocardiogram is performed to confirm the severity of the leakage and the suspected mechanism for the leak. A referral to our Advanced Structural and Valvular Heart Disease program can provide you with an evaluation by our Heart Team of cardiologists, cardiothoracic surgeons, and echocardiography experts. We will carefully review your echocardiogram and decide whether you should be considered for surgery. This may require a transesophageal echocardiogram at Saint Vincent to obtain a better assessment of your mitral valve. If surgery is not feasible, but the anatomy appears favorable for a MitraClip, we will then meet with you to discuss the nature of the procedure, and its risks and benefits.
Preparing for the MitraClip Procedure
 The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.
The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.
Results of MitraClip
The MitraClip procedure has been successfully implanted in just over 90% of patients and the degree of MR has been reduced to moderate or less in degree in 90% of patients. The long-term results are not known, since this is relatively recent technology, but the significant reduction in MR in most patients should lead to an improved quality of life and most likely increase longevity.
Our specialized team of providers will arrange all of your appointments, schedule pre-admission testing, perform the procedure, follow you throughout your hospitalization, and arrange follow-up appointments after discharge.

 Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing.
Surgery is the most effective means of eliminating significant MR, improving symptoms, and improving long-term survival. Mitral valve repair is preferable for patients with "degenerative" MR, whereas mitral valve replacement may be best for "functional" MR. However, some patients will have congestive heart failure from severe leakage but are considered too high risk to tolerate surgery. These include very elderly patients, those with multiple other medical problems, and patients with severely decreased heart muscle function. The MitraClip system is a means of improving valve leakage without open-heart surgery. Using access through the femoral vein in the groin, a catheter is passed into the heart and across the muscle between the upper two chambers. The device is then advanced across the mitral valve, and two clips grasp the anterior and posterior leaflets of the valve to bring the leaflets together at the same plane. This creates a double-inlet into the left ventricle with reduction in the leak with minimal narrowing. The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.
The procedure is performed in our new hybrid cath lab which provides state-of-the-art technology. It is performed under general anesthesia which allows us to perform a transesophageal echocardiogram during the implantation which can take several hours. During preadmission testing, you will meet with an anesthesiologist who will review your history, medications, and lab tests. Some patients require admission the day before the procedure, especially those on anticoagulation, while others may be admitted the morning of the procedure. Instructions on preparing and arriving for the procedure will be given to you in advance.